Cardiac Surgery (CABG)
CARDIAC SURGERY
Why Heart Surgery?
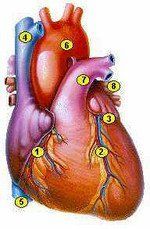
Structure and Function of the Heart:The heart is a four-chambered, hollow, muscular organ. It is located within the chest, behind the breastbone (sternum) and slightly to the left. It is the size of one's fist, and it weighs less than one pound. The heart's job is to pump blood to every part of the body. The AORTA and ARTERIES carry oxygen and nutrient-enriched blood away from the heart to all the cells of the body. The VEINS then collect the blood from these cells and carry it back to the right side of the heart.
The two upper chambers of the heart are called the right and left ATRIA . The right atrium receives the venous blood from the body. The left atrium receives the blood from the lungs. The two lower chambers are called the VENTRICLES . These muscular chambers pump blood out of the heart. The right ventricle pumps venous blood only to the lungs. In the lungs, the red blood cells pick up oxygen, and the oxygenated blood is pumped to the remainder of the body by the left ventricle.
There are four VALVES present within the heart. These valves act as one-way doors to prevent the backflow of blood. A wall called the SEPTUM divides the heart into right and left sides.The heart is the hardest working muscle in the body. For this reason, it requires a continuous supply of oxygen and nutrient-enriched blood. The heart muscle receives its blood supply from the CORONARY ARTERIES. There are three primary coronary arteries, and each one has many smaller branches, allowing every portion of the heart to receive blood. The right and left main coronary arteries originate from the aorta.
The three primary arteries include:- Right Coronary Artery- supplies blood to the right half of the heart.
- Left Anterior Descending Artery- supplies blood to the front portion of the heart muscle.
- Left Circumflex (LCx) Coronary Artery- supplies blood to the left side and back of the heart.
Coronary Arteries and Great Vessels
1. Right Coronary 2. Left Anterior Descending 3. Left Circumflex 4. Superior Vena Cava 5. Inferior Vena Cava 6. Aorta 7. Pulmonary Artery 8. Pulmonary Vein
Coronary Artery Disease:Blockages can occur in the coronary arteries, decreasing the amount of blood flow to the heart muscle. The most common cause of blockages is fatty deposits (atherosclerosis) accumulating in the walls of the coronary arteries. This accumulation of fatty deposits is thought to be influenced by numerous risk factors that include:- Smoking
- Cholesterol
- High Blood Pressure
- Diabetes
- Male Gender
- Heredity and Age
- Non-Traditional Risk Factors and Markers: Lipoprotein(a), Homocysteine, C-reactive protein.
To determine your 10-year risk of developing coronary heart disease, take the Heart Attack Risk Test.
As deposits continue to build within the arterial wall, the internal diameter of the vessel decreases, blockage results, and the blood supply to the heart muscle is jeopardized. This often results in chest pain known as ANGINA. Anginal pain is usually relieved by nitroglycerine and rest.
If blood flow through a coronary artery becomes severely reduced, a portion of the heart muscle becomes damaged and may die-- known as a Myocardial Infarction (MI) or heart attack. MI's are felt to be a consequence of blood clot formation (plaque rupture and thrombosis) in a coronary artery.
Coronary Angiogram:The Coronary Angiogram is the cornerstone of a left heart catheterization (or cardiac "cath"). This test is used to determine the location and severity of any blockages present in the heart's arteries, and assesses the function of the heart valves. During the test, a small amount of dye is injected into the coronary arteries, and is recorded digitally using X-ray imaging. Dye is also injected into the left ventricle of the heart to establish whether any damage has occurred to this muscle or to the heart valves.
The cardiologists and cardiovascular surgeons will look at the results of the cardiac catheterization films and decide if open heart surgery is needed or if an alternative method of treatment can be used. Alternative methods of therapy include coronary angioplasty (PTCA), rotational atherectomy, and coronary stenting. The recommended treatment will depend upon your personal medical history, the anatomy of coronary artery disease that is present, and your individual needs.
Coronary Artery Bypass Surgery:Coronary artery bypass surgery restores blood supply to various areas of the heart muscle. This is done by attaching one end of a saphenous vein segment (which is removed from the leg) to the aorta, and the other end of the vein just beyond the point of blockage in the coronary artery. The blocked portion is not removed. This vein graft will now deliver an increased blood supply to the heart muscle that lies beyond the point of blockage. The internal mammary artery, which courses inside the chest wall, is also used as a bypass graft conduit.Cardiac Chamber and Valves
9. Right Atrium 10. Right Ventricle 11. Left Atrium 12. Left Ventricle 13. Papillary Muscles 14. Chordae Tendineae 15. Tricuspid Valve 16. Mitral Valve 17. Pulmonary ValveAortic Valve (Not pictured)
Heart Valve Replacement Information:The heart has four Valves:- Aortic
- Mitral
- Tricuspid and Pulmonic
These one-way valves separate the heart chambers from one-another and from the "great vessels" and keep blood flowing properly. Diseases such as rheumatic fever, infection, atherosclerosis, or birth defects may cause the valves to leak or become obstructed. Depending on the extent of valve damage, surgery may be advised to either repair or replace the valve.
Prosthetic, or replacement, valves come in two flavors, mechanical (metal) and bioprosthetic (from living tissue). The mechanical valves are especially durable and require long-term therapy with blood thinners (anticoagulants).
To learn more about Coumadin (warfarin) anticoagulant therapy, visit our Coumadin Clinic Information page.
The tissue valves are not quite as durable as their mechanical counterparts, but typically don't require blood-thinning. The decision on what type of valve to implant is arrived at jointly by considering your needs and the recommendations of your cardiologist and cardiovascular surgeon.
- Right Coronary Artery- supplies blood to the right half of the heart.
- Left Anterior Descending Artery- supplies blood to the front portion of the heart muscle.
- Left Circumflex (LCx) Coronary Artery- supplies blood to the left side and back of the heart.
- Smoking
- Cholesterol
- High Blood Pressure
- Diabetes
- Male Gender
- Heredity and Age
- Non-Traditional Risk Factors and Markers: Lipoprotein(a), Homocysteine, C-reactive protein.
- Aortic
- Mitral
- Tricuspid and Pulmonic
Corporate Offices
13011 S. 104th Avenue
Suite 100 | Palos Park, IL 60464
P:
708.478.3600
F: 708.478.3552
CONTACT US
This form is intended for non-patient related questions. For any patient related needs or to schedule an appointment, please call 888.642.4224
Footer Contact Form
Thank you for contacting us.
We will get back to you as soon as possible
We will get back to you as soon as possible
Oops, there was an error sending your message.
Please try again later
Please try again later
CLINIC LOCATIONS
-
Berwyn
MAP IT3231 South Euclid Ave
Suite 201
Berwyn, IL 60402
P: 708 783 2055
F: 708 783 2181
-
Hinsdale
MAP IT911 Elm Street
Suite 328
Hinsdale, IL 60521
P: 708 608.8588
F: 708 608.8589
-
Joliet
MAP IT2121 Oneida St
Suite 202
Joliet, IL 60435
P: 815 823 8200
F: 815 823 8201
-
Merrionette Park
MAP IT11560 S. Kedzie Ave
Suite 100
Merrionette Park, IL 60803
P: 708 824 1114
F: 708 824 9341
-
Mokena
MAP IT10260 West 191st St
Suite 102
Mokena, IL 60448
P: 708 478 4224
F: 708 478 4033
-
Palos Park
MAP IT13011 S. 104th Ave
Suite 100
Palos Park, IL 60464
P: 708 274 3278
F: 708 274 3299
Heart Care Center of Illinois | All Rights Reserved |
Created by Olive + Ash.
Managed by Olive Street Design.